Patient-Reported Experience Measures (PREMs) and Patient-Reported Outcome Measures (PROMs) are terms that are easily used and sound the same. However, even though they are complementary, they are also very different, especially when we consider what they measure and can achieve when used effectively.
In this article we look at how PREMs and PROMs can work together.
Patient-Centred Care
There is increasing recognition for the importance of the patient’s perspective in supporting a patient-centred approach to providing quality health care.
- How many patients have had a good experience from the care they were provided?
- Did the patients achieve their goals and desired outcome?
- Do we know if the current care pathway and treatment is best suited for these patients?
- What can we do to improve their experience and their health outcomes?
These important questions can only be answered completely and effectively by the patient themselves or the people and carers closest to them.
Understanding the patient’s view of their experience following treatment or procedure as well as their perspective concerning their health status and ongoing quality of life are essential components for patient-centred care, quality improvement and organisational performance.
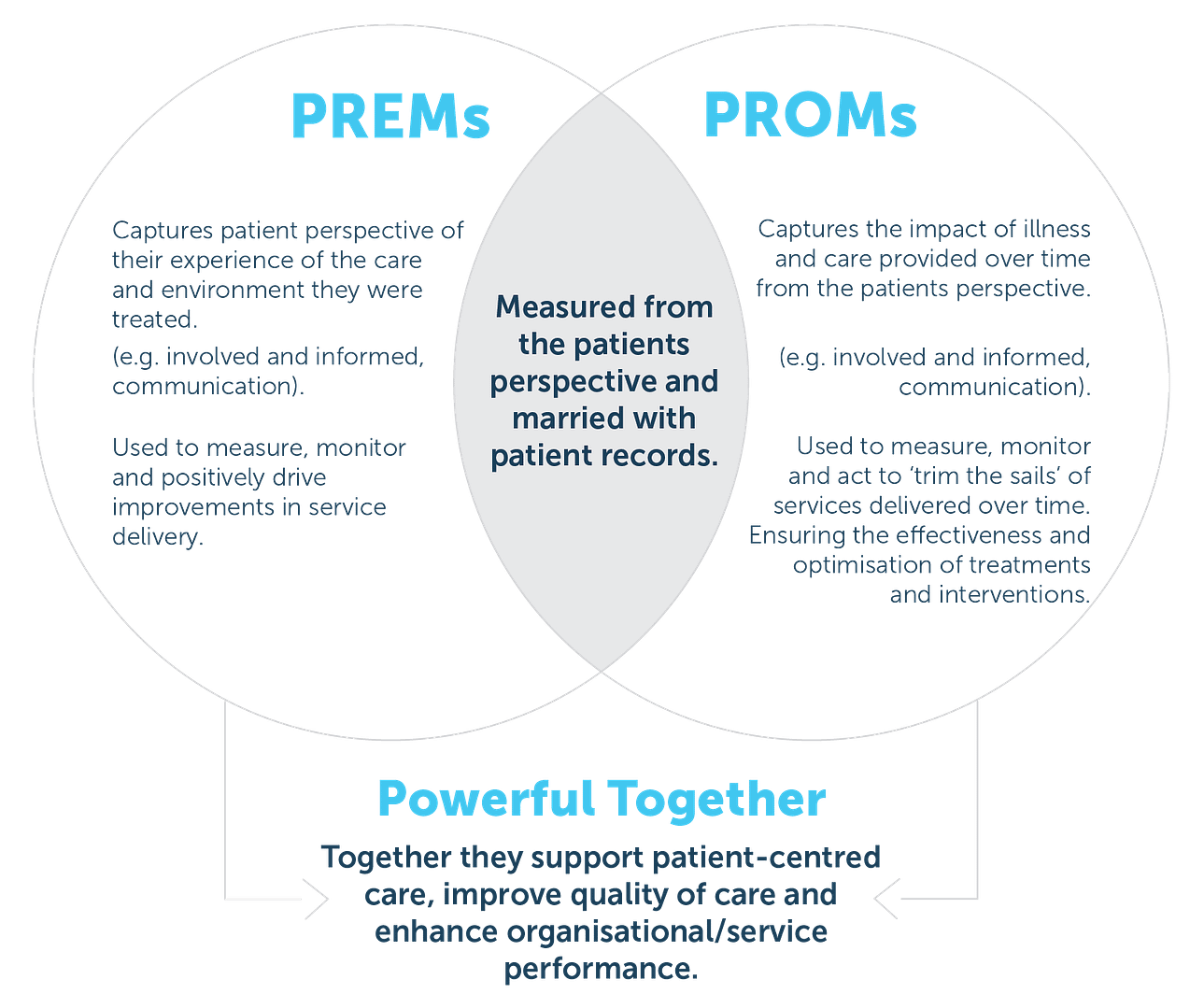
Explaining PROMs and PREMs
To understand how they can work together, we need to establish the difference between experience and outcomes. PREMs asks patients about their experience of care, typically utilising validated survey tools that focus on the core drivers of a good patient experience. By patients sharing this with us, we can recognise, celebrate or address the patient journey and care pathway for future patients. This information enables health organisations to measure, monitor, evaluate and act on these insights to continually improve what they do going forward. They are designed to support quality improvement and benchmarking across an organisation, region, or country.
PROMs capture the impact of illness, health condition, symptoms, or side-effects from the patient’s perspective. They are used to assess a patient’s health status at a particular point in time, over a period of time. PROMs are completed before, during and after the treatment for a health condition. Ideally, PROMs are collected pre and post-event to help measure the impact of an intervention, for example radiation and medical oncology, stroke and chronic rheumatoid arthritis.
PROMs are increasingly being recognised as providing valuable and essential benefit to patients in their care and have been shown to provide significant improvements in both quality of life and survival rates.
For example, In 2015 Bache et al [1], used a real-time PROMs for patients with advanced breast cancer to enable patients to track and report their symptoms remotely, sending alerts to their nurse carer when symptoms were concerning. Patients reported significant and clinically meaningful improvements in quality of life, there were fewer hospital admissions and an increased adherence to treatment. Amazingly the median overall survival was 5 months longer in the ePRO group than in the usual care group, a stronger impact than many new cancer drugs achieve.
The evidence showed that from both a clinical and a business case perspective, using PROMs achieved better outcomes for patients, enabled better use of clinic time and reduced pressure on thinly spread oncology nurses and busy clinics.
Research continues to demonstrate quality of life benefits of PROMs in both acute and chronic conditions such as other forms of cancer [2], stroke [3], orthopaedics [4], cardiology [5], rheumatology [6], respiratory [7].
Both PROMs and PREMs are measured from the patient’s perspective, and they can be used together to assess quality of care more fully, and the value of health services delivered. Information from the patient’s perspective is essential to supporting a patient-centred approach to care, as outlined in CIHI’s Health System Performance Measurement Framework.
PROMs can also complement traditional sources of data, such as information derived from clinical administrative data, to inform policies, programmes, and value-based health care delivery. They are essential to understanding whether health care services and procedures make a difference to patients’ health status and quality of life. The diagram below shows the individual roles, and combined benefit of PREMs versus PROMs.
Capturing PROMs alongside traditional clinical outcomes can offer a range of benefits: at an individual patient level PROMs can facilitate communication, identification of problems and help tailor care to needs.[1][8][9]
Value Based Healthcare
A healthcare system that is patient-centric is also value-based. But what does value-based healthcare really mean? According to the NHS in the UK, value-based healthcare is the equitable, sustainable, and transparent use of the available resources to achieve better outcomes and experiences for every person.[10]
Value-based healthcare, is healthcare that delivers the best possible outcomes to patients for the lowest possible cost.[11] It looks at the available resources, expertise, skills, techniques, medications, technology and systems aimed in a coordinated and dynamic way to provide the best possible outcomes for every patient. Yet, one of the most important components of this approach continues to be considered in isolation and separately as an alternative or novelty. Digital technology has enabled the voice and perspective from the patient to be available in real-time to the people who can do something with it and make a quantifiable difference.
Patients are considered more like partners in a patient-centred and value-based healthcare environment. Providers treat patients not only from a clinical perspective, but also from an emotional, mental, spiritual, social, and financial perspective. Increasing evidence and experience demonstrates the use of PREMs and PROMs together can provide the most effective method to engage, capture, and utilise the powerful insights gained from these important ‘partners’.

