Due to the plethora of evidence of the value of transitioning from fee-for-service to value-based funding mechanisms in healthcare, funders/payers are increasingly looking to mechanisms providers are paid based on patient health outcomes. Effectively, this means that rewards are given for helping patients improve their health, reducing readmission rates, adhering to medicine and feeling like the result of the process has led them to a better quality of life.
However, the path to value-based health care can be long and arduous. Most health systems remain largely measured by key performance indicators (KPIs) and clinical metrics; at present little attempt is made to understand patients’ perspectives of their health outcomes.
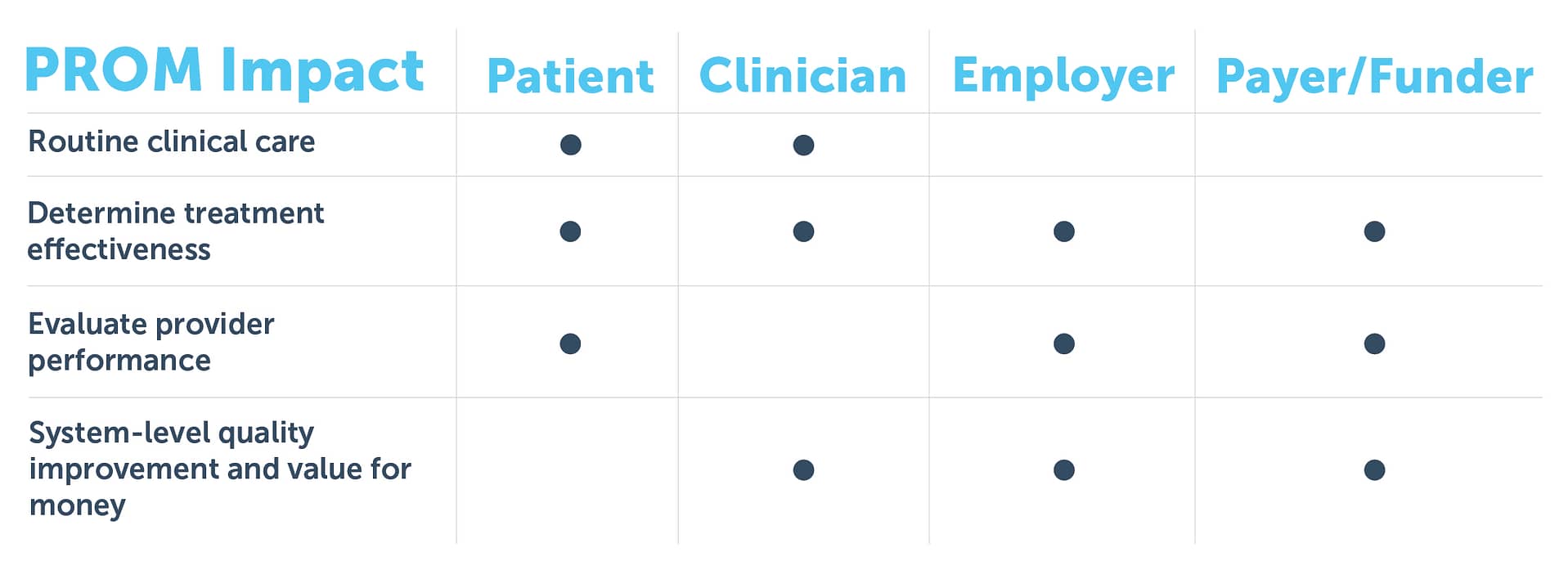
One of the biggest challenges to date has been the implementation of Patient-Reported Outcome Measures (PROMs) that meets the need of all stakeholders. The objectives of stakeholders are significant, varied and at times, conflicting. However, we know each should be catered for to some extent to truly deliver a value-based care model – the table below gives you some indications of which elements of PROMs suit each key stakeholder:
However, while complex, here at Cemplicity we have seen PROMs delivered at scale that met the primary needs of all. Importantly, this is only achievable if you leverage the latest advances in PROMs technology to streamline the process. Specifically:
- Reaching patients at home – digital channels for feedback – whether it be email, text, apps or home-based tablet devices – enable patients to talk about their own health in their comfort of home. This not only gives the patient more time to consider their responses, it enables genuine tracking of health outcomes when the patient is not physically on-site with the clinical team.
- Patient defined outcomes – there is, understandably, a lot of focus on validated tools when discussing suitable PROMs measures. However, technology can supplement this with patient-defined metrics to bring even greater focus to what each individual patient needs. A great example of this is asking each patient their “Goal for Treatment” as a baseline and asking them to review progress against this goal in subsequent data points.
- Smart survey logic – patients with multiple chronic conditions may feel inundated with excessive surveying. Modern PROMs platforms can alleviate this by embedding multiple condition PROMs into a streamlined survey experience for the patient without the need for multiple forms and repetition.
- Real-time access to results – getting the data to your patients and clinicians for routine clinical care instantly is a key metric of success. In real terms, if a patient fills in a survey in the waiting room, it must be available to their clinician before they walk into their room. That means real-time reporting capability.
- Instant alerts – specifying thresholds based on patient responses, and in turn alerting clinical teams when those thresholds are triggered, immediately engages patients in the value of their feedback, and provides important information to clinical teams about how that patient is feeling today, particularly while they are home.
- Cloud-based analytics – using the internet and role-based access, different stakeholders can easily access the data within a secure environment that suits their specific needs.
- Collective wisdom – technology platforms such as “Software as a Service” use the same code-base for all their clients. This means all clients using that platform are sharing the same functionality, albeit at times configured differently. This provides a collective ‘backstop ’ of accuracy and robustness across the system functions. It is particularly relevant in the analytics capability i.e. you get comfort while evaluating and using the solution, that many others have already tested it before you, and using the solution actively in clinical practice.
A fully realised value-based care model delivers the patient voice at all levels within the organisation, all the time. As in many systems today, technology has provided great solutions in progressing funders and payers towards that value-based care model. I encourage you to explore the learnings outlined in this blog to see how they can truly streamline, and bring genuine patient outcome data, into your value-based care model.

