I spend much of my time talking to clinicians and hospital managers about the benefits of asking patients about their own health through patient reported outcome measures programmes. However, we also encounter scepticism that, by enabling patients to rate their own health, better outcomes will be achieved. A new study, Basch (2017 pp.197-198), shines a clear light on the fact it is not whether you should implement PROMs, it’s how you implement it that will have the impact. Frustrated frontline teams who understand the value of patient feedback yet who cannot secure the budget or management attention for patient reported outcome measures need look no further than this new study.
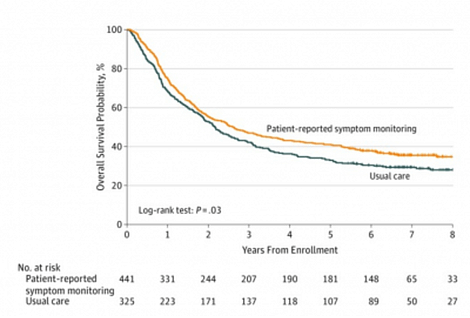
Basch looked at the ‘Overall Survival Results of a Trial Assessing Patient-Reported Outcomes for Symptom Monitoring During Routine Cancer Treatment’. This study shows how electronic patient-reported outcome measures for cancer patients can improve patient comfort, unplanned readmissions and other benefits that come from real-time patient feedback programmes. This study also shows that survival rates for cancer patients were increased by 10% by this real-time patient reported outcome measures approach (see image below), a stronger impact than most new cancer drugs achieve.
Image: Increased survival probability in Patients with Metastatic Cancer assigned to Electronic Patient-Reported Symptom Monitoring vs those receiving normal care during routine Chemotherapy (Basch, 2017).
Cemplicity staff take an interest in all robust patient reported outcome measures research and the Basch study is getting significant attention because of the large patient sample, the length of the study (8 years), the credibility of the sponsoring institute (Memorial Sloan Kettering Cancer Centre in New York), and the reputation of the author, Ethan M. Basch, MSc, FASCO, Professor of Medicine at the Lineberger Comprehensive Cancer Center of the University of North Carolina.
The research enabled 766 patients to report their symptoms electronically. When alarming results were entered, an automated email alert was sent to the clinical nurse responsible for that patient’s care. Importantly, every treating oncologist also had real-time access to each patient’s symptom history either prior to or during treatment and consultation. The control ‘usual care’ group discussed symptoms only with their oncologist in the normal manner.
Arguably, the most important aspect of this study is the proof that the patients’ symptoms were better managed. Mr Basch commented that “patients receiving chemotherapy often have severe symptoms, but doctors and nurses are unaware of these symptoms up to half of the time”. The timeliness of this patient reported outcome measures approach and the direct reporting to clinicians was key to the good outcomes achieved in this area of symptom management.
Beyond better patient outcomes, this study also highlighted the benefits at a health service or system level. There were less visits by patients to emergency department, fewer unplanned hospital visits generally and fewer unscheduled reductions in chemotherapy programmes.
We were particularly impressed by the finding that in almost every case where a real-time alert was triggered by patient self-reporting symptoms, the nurse changed something. They either counselled the patient on symptom management, changed medication, or referred the patient to the hospital. Not only did this help the patients feel better, it meant they continued their chemotherapy treatments 33% longer than the control group. This is felt to be a key reason why survival rates went up. This level of staff engagement is essential for a successful programme.
Cemplicity has implemented real-time, continuous patient feedback systems across four countries and many different health settings. What interests us about the efficacy of the approach Basch has evaluated is that it includes each of Cemplicity’s “4 Pillars” for best practice patient feedback programmes. There is plenty of evidence that patient feedback on their experiences and health is important in any patient-centred health system. However, it is how you run your programme that will determine its impact. You can read about the 4 pillars we consider to be best practice when designing a patient experience programme.
The Basch study convincingly presents the case for patient reported outcome measures for cancer patients, as well as valuable insight into how to run an effective programme. I hope it brings a greater sense of urgency and removed roadblocks for teams considering whether or not PROMs would improve the outcomes for their patients. Comments welcome!